Dupuytrens Disease
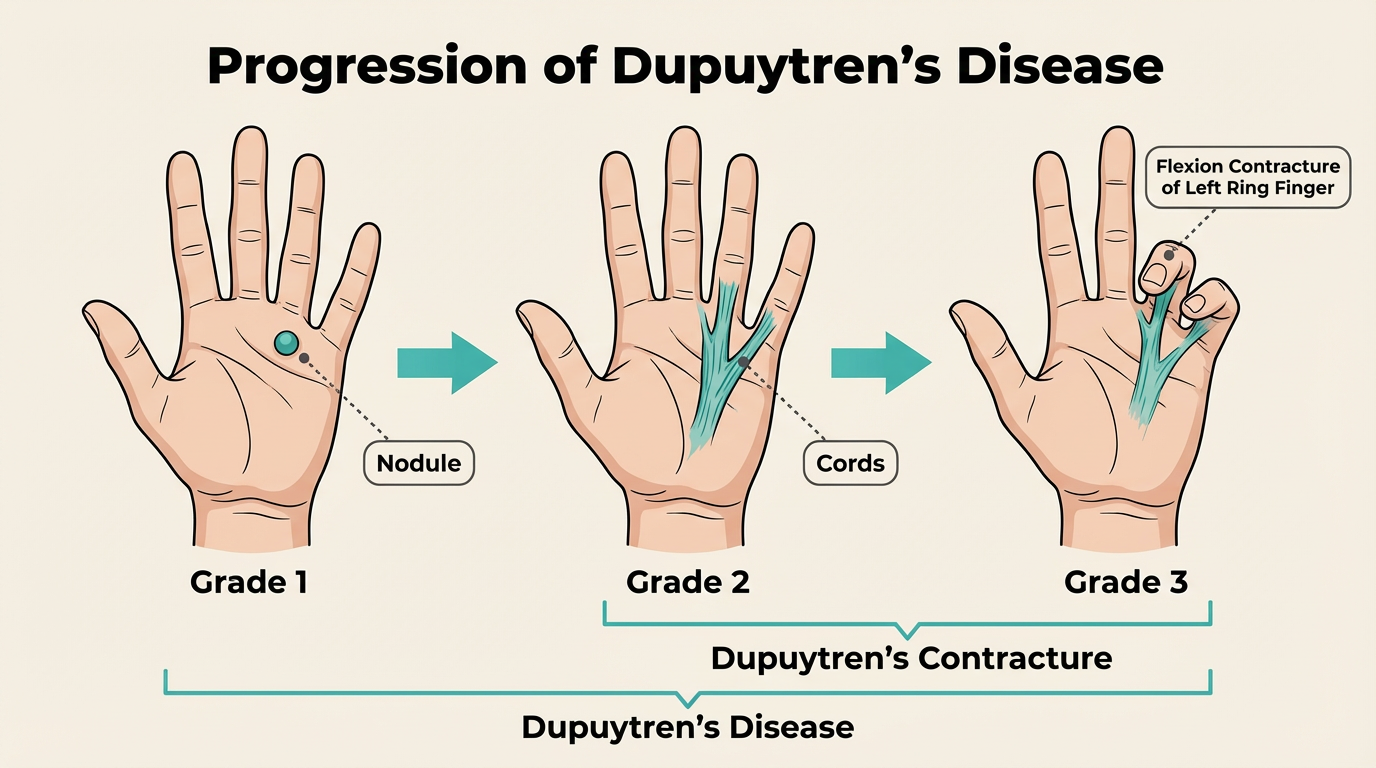
This is a common condition that usually arises in middle age or later and more common in men than women. Early disease is characterised by firm nodules in the palm just beneath the skin, and can extend into cords causing the fingers start to contract down, preventing the fingers from straightening.
The nodules/cords can be associated with small pits in the skin, nodules over the back of the finger knuckles (Garrod’s pads), or lumps on the soles of the feet (Ledderhose disease). In men, it can affect the penis – Peyronie’s disease.
Cause
The cause is unknown but more common in Northern Europe and in populations with Viking descent. It may be associated with diabetes, smoking, alcohol or previous trauma, but most affected people have none of these associations. It does not seem to be strongly associated with manual work.
Symptoms
The first sign of the condition is often a nodule or lump in the palm of the hand, often in line with the ring finger. The nodules can occasionally be painful in the early days but this discomfort normally settles. In one out of three people affected, the condition progresses and a cord may become evident. This is often mistaken for a tendon, but in fact the tendons are not involved in this condition. Patients with moderate or severe Dupuytren’s may have extensive diffuse lumps in the palm, fingers and occasionally the thumb. This condition can take years to develop.
Treatment
Dupuytren’s disease is not a serious problem. It is NOT a type of cancer. It may affect up to 2 million people in the UK, but only a small amount of people require surgery.
Many people do not find that the condition affects their function, and do not require treatment. If you are able to get your hand flat on the table, none of the treatment options outlined below are likely to be of any benefit to you. However, if the contracture is beginning to interfere with the function of your hand, for example having problems putting your hand in a pocket or glove, or holding tools, then discussion with a specialist may be a good option.
There is no cure. Surgery can usually make bent fingers straighter, though not always fully straight; it cannot eradicate the disease. Over the longer term, Dupuytren's disease may reappear in operated digits or in previously uninvolved areas of the hand but most patients who require surgery need only one operation during their lifetime.
Treatment options
The surgeon can advise on the type of operation best suited to the individual, and on its timing. The procedure may be carried out under local, regional (injection of local anaesthetic at the shoulder) or general anaesthetic.
Needle fasciotomy
This is a Day Case procedure. A local anaesthetic injection numbs the area and allows the surgeon to divide the Dupuytren’s cord at multiple levels with a needle through the skin. It is only suitable if the cord is pulling from the palm rather than at the finger, since the risk of nerve and vessel damage becomes too high when the disease is past the crease at the base of your finger. The contracture usually improves, but may not come fully straight. Recovery is very fast, but there is a higher recurrence rate (i.e. chance of it returning) than with other techniques.
Open Fasciotomy
This is usually performed under a general anaesthetic and involves a cut in the palm of your hand with a small knife in your palm or finger or both. This leaves an open wound (without stiches) which will need to be kept clean and dry until it heals, up to 4 weeks later.
Open Fasciectomy
This involves a general anaesthetic with an incision along the length of the finger, to allow the entire cord to be removed safely. This is the most common operation we perform for Dupuytren’s. Part of the palm wound may be left open, and this can take around 4 weeks to heal.
Dermofasciectomy
Under general anaesthetic, the cord is removed together with the overlying skin. The skin is replaced with a graft (when a healthy piece of skin is taken from another part of the body, usually the forearm). This procedure is undertaken for recurrent disease, or for extensive disease in a younger individual. A plaster cast is required for the first 7-10 days after surgery and the palm wound is sometimes kept open, again requiring about 4 weeks to heal.
Amputation
Amputation of the finger may be an option in very severe or recurrent Dupuytren’s in the finger. This is very unusual and requires a full discussion with the specialist.
Following Surgery
After surgery, the hand may be fitted with a splint to be worn at night.
Most patients return home on the same day.
Hand therapy is important in recovering movement and function, especially for more extensive surgery and skin grafts.
The recovery is variable with regard to the degree of improvement achieved and the time to achieve the final position.
The final outcome is dependent on many factors including the extent and behaviour of the disease itself and the type of surgery required.
Complications
There are a number of complications that can occur after these techniques:
Scar: on the finger, palm and upper arm (if skin graft is required).
Infection: this would usually be treated with antibiotics.
Nerve damage: the two nerves on either side of the finger can get damaged (more common in repeat operations) which may lead to some permanent numbness on one (or both) side(s) of the finger.
Recurrence: Dupuytren’s Contracture can never be cured. It can return at the site of surgery or elsewhere in the hand.
Bleeding: this can cause a collection of blood under the stitches, which can cause a problem with the wound. Occasionally this requires further surgery, or removing the stitches a bit earlier than planned. Inform the surgeon if you are on warfarin, aspirin or clopidogrel.
Stiffness: about 5% (1 in 20) people develop ‘chronic regional pain’ in the hand following hand surgery and the hand becomes stiff, painful and swollen after the operation. This is treated with physiotherapy and analgesics (pain relief).
Residual deformity: it is often not possible to fully straighten the fingers at the time of the operation, particularly if the bend is in the middle of the finger (proximal interphalangeal joint).
Skin loss: portions of the zigzag scars and skin grafts can “die”. This is unusual provided you don’t smoke and follow all the advice given.
Finger loss (amputation): this is rare, but can occur in fingers which have had many previous operations and in patients who have diseases of blood vessels such as diabetes or scleroderma.
Alternative Treatments
Steroid injections: These injections may help with local tenderness, but have no significant effect on the disease and are not recommended.
Xiapex injection: This drug has now been withdrawn from the market.
Radiotherapy: Radiotherapy is an experimental treatment offered in some research centres, but is not available on the NHS