Knee Osteoarthritis
Osteoarthritis is a normal age related condition that causes joints to become painful and stiff. The knee is one of the joints most affected by osteoarthritis. The aim of this webpage is to provide you with information about the problems faced with age related changes in your knee and suggest a few helpful hints on how to help manage your symptoms.
The Knee
The knee is one of the largest joints in the body. It acts as a hinge and withstands a lot of twists and turns in our everyday life. If you are active and play sport, you will need your knee to be as strong as possible to meet your sporting demands.
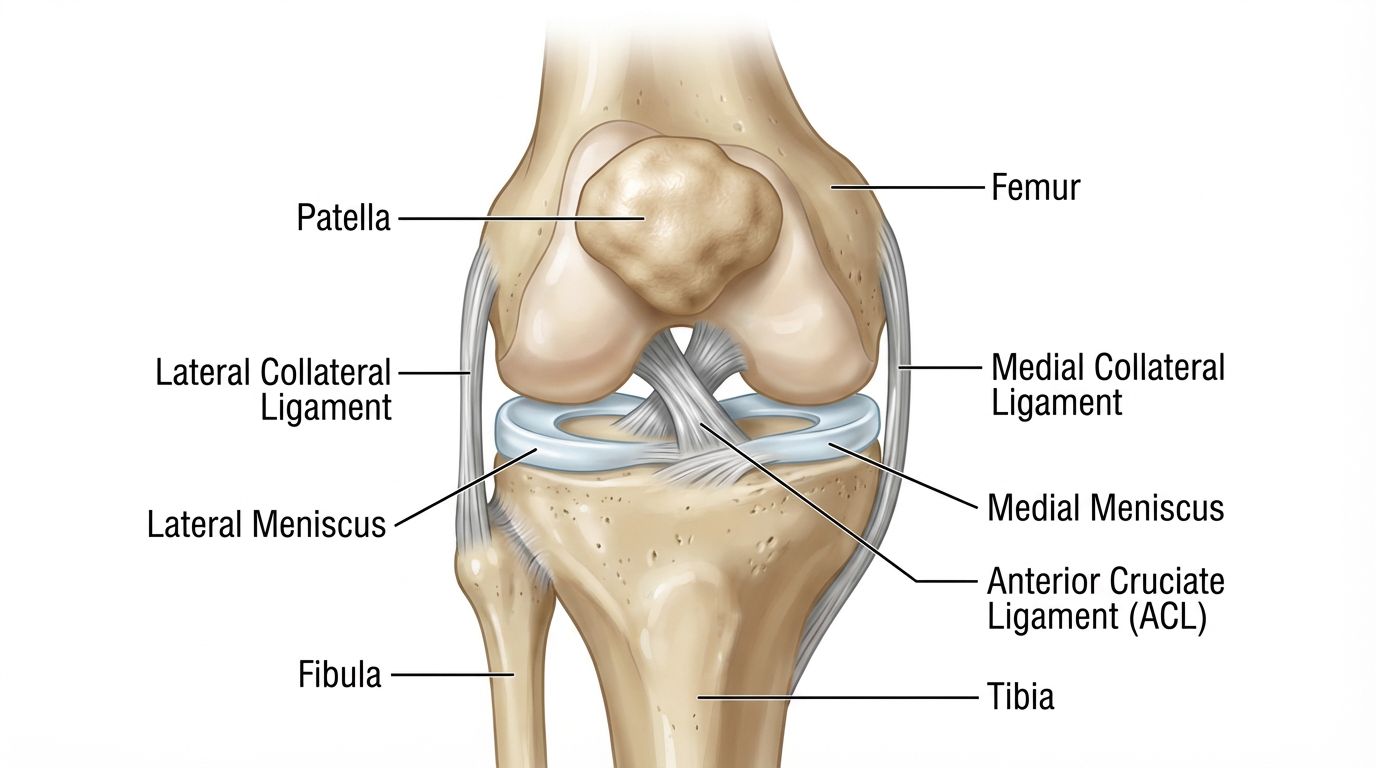
Bones
The knee joint is formed by three bones – the thigh bone (FEMUR), the large shin bone (TIBIA) and the knee cap (PATELLA). The smaller shin bone (FIBULA) is also closely linked, but is not part of the knee.
Ligaments
Four large and strong ligaments keep the knee joint stable, two outside the knee joint (MCL/LCL) and two inside (Cruciates ACL/PCL).
Cartilage
There are also two cartilage structures, also known as Menisci, inside the knee which help to keep it stable and provide some shock absorption.
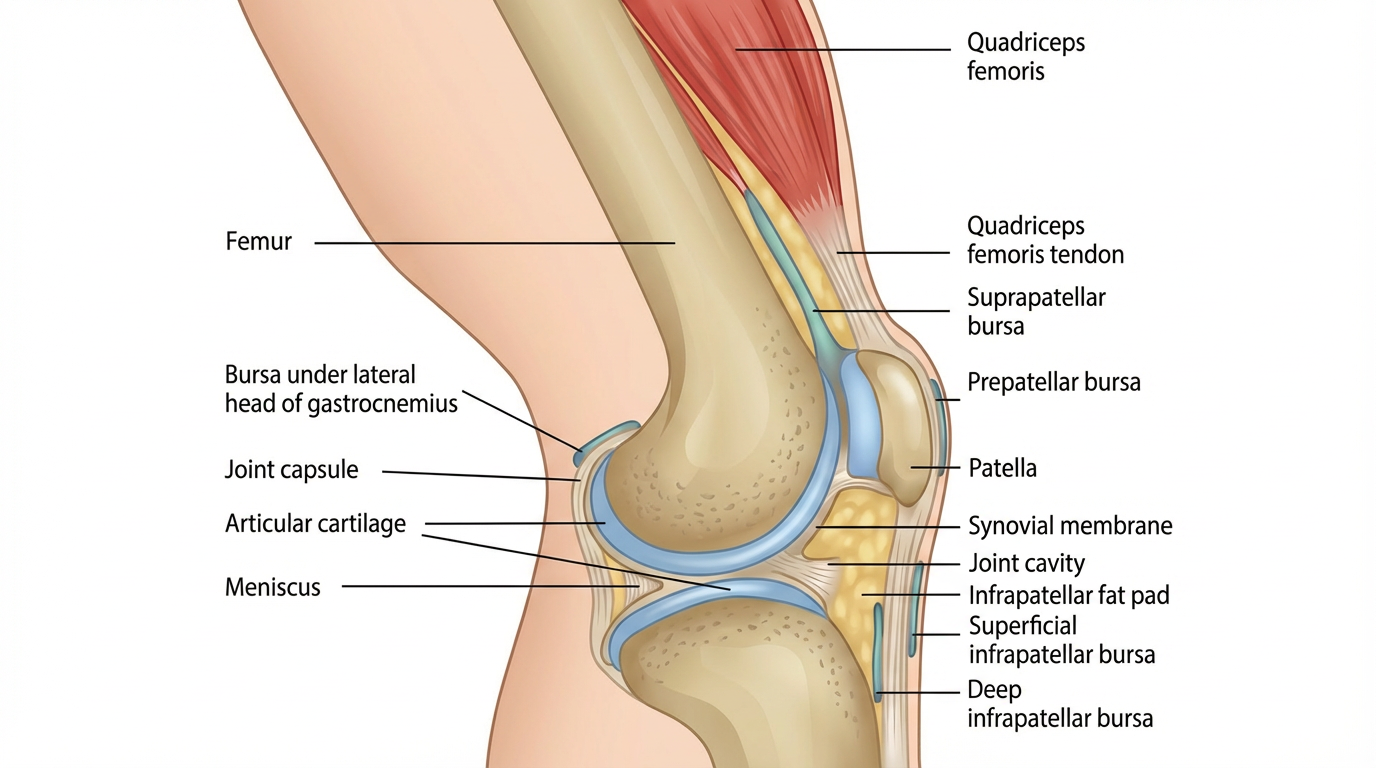
Muscles
To provide movement at the knee, muscles attach to the bones by strong connecting tissues called tendons. These muscles also provide further support and can also reduce the forces going through the knee. These muscles are:
The Quadriceps (at the front of the thigh)
The Hamstrings (at the back of the thigh)
The Gastrocnemius and Soleus (large Calf muscle)
Joint capsule
Each joint also contains synovial fluid, which acts as lubricant to reduce friction as we move. The more we move, the more synovial fluid is distributed across the joint surfaces lubricating the joint, and also explains why we stiffen up if we keep still for too long.
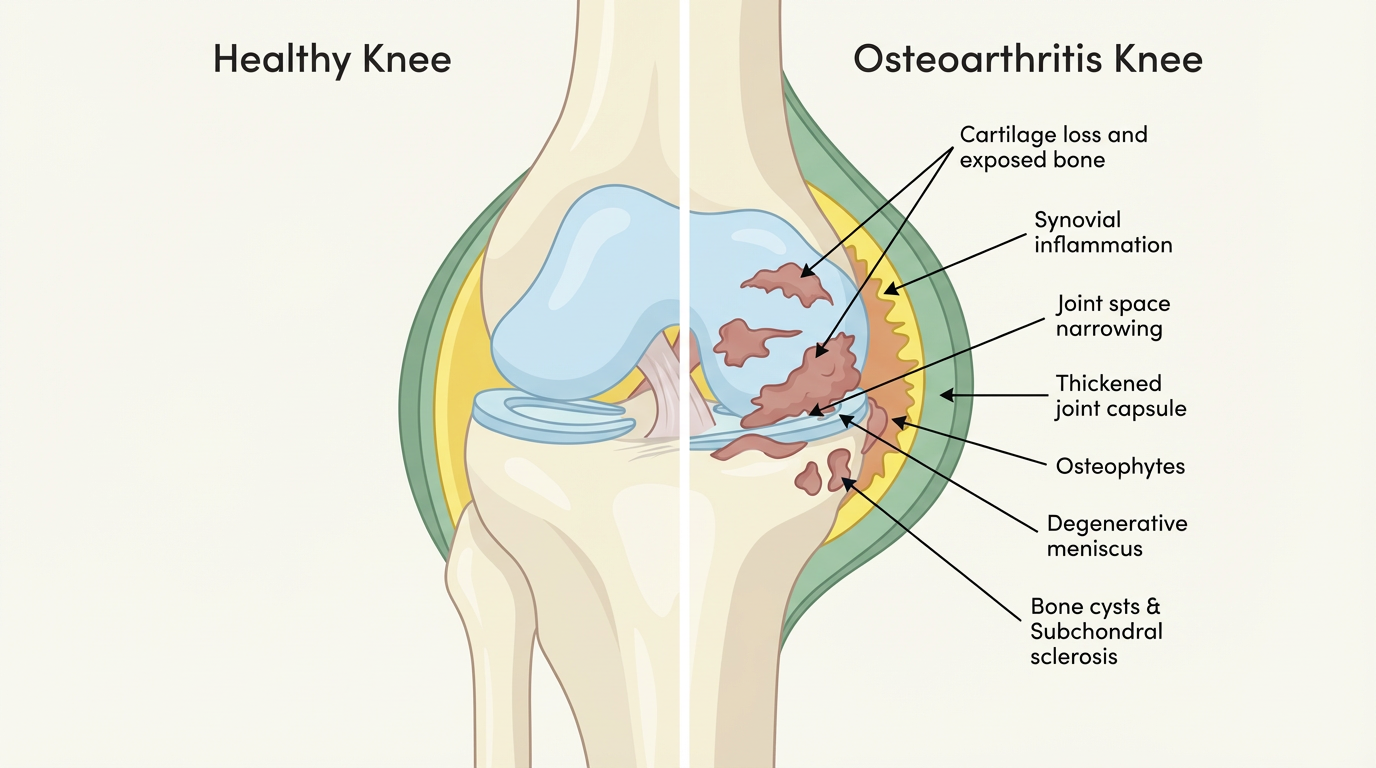
What is knee OA (age related knee pain)?
Osteoarthritis is a normal age related change that occurs in the joints. When a joint develops osteoarthritis, it affects the cartilage covering the ends of the bones and can cause the development of bony spurs called osteophytes. Additional changes occur to the synovial fluid, causing stiffness in the joint and occasionally the joint space begins to narrow which can further reduce the movement of the joint.
These changes in and around the joint are partly the result of the inflammatory process and partly your body’s attempt to repair the changes which have occurred.
This process is a perfectly normal part of ageing and happens in all joints but tends to happen earlier in joints that carry a lot of weight through them. This is why the knee, and also the hip, are most commonly affected. In many cases there is no pain, however, as this process continues it can increase symptoms of stiffness and pain to become more severe and persistent.
What are the symptoms of osteoarthritis?
The symptoms of osteoarthritis can include:
Pain
A grating or grinding sensation when the joint moves (crepitus)
Swelling (either hard or soft).
Sometimes the knee may either lock or give way when you put weight on it.
Weakness and wasting of the quadriceps muscles at the front of your thigh
Loss of range of motion, particularly when bending and straightening the knee
Stiffness around the knee, making movements slower or more difficult.
Trouble going up stairs. Changes to the knee’s range of motion may change a person’s natural gait while climbing stairs.
A loss of balance. Balancing on the affected leg may be more difficult than balancing on the unaffected leg.
Limping. In moderate to severe cases of knee OA, knee pain and other symptoms may cause a person to find walking difficult and can lead to a limp. It is important to try and avoid limping, to allow the joint to move through its full natural range of movement.
Who gets it?
Almost anyone can get osteoarthritis, but it’s most likely if:
You’re in your late 40s or older. Remember it is a normal age related change to the joint surface.
You’re overweight: Being overweight is an important factor in causing osteoarthritis, especially in the knee. It also increases the chances of osteoarthritis becoming progressively worse.
You’re a woman: twice as common in woman as in men.
Your parents, brothers or sisters have had osteoarthritis
You’ve previously had a severe knee injury: repetitive activity or physically demanding jobs can increase the risk. Previous injuries to the ligaments or meniscus including surgery can increase the risk of arthritis.
Your joints have been damaged by another disease, for example rheumatoid arthritis or gout.
What can I do to help myself?
There are several ways you can help yourself, including:
Losing weight if you’re overweight
In fact, evidence shows that weight loss through exercise and a healthy diet may reduce your pain and improve your general lifestyle. Losing weight also helps improve your mood, reduces inflammation in the body, can lead to improved sleep and reduces the risk of other diseases.
Exercising regularly (both muscle-strengthening and general aerobic exercise)
Using painkillers (analgesics) or anti-inflammatory creams, gels and tablets.
Reducing stress on the affected joint (for example by pacing activities, using a walking stick or wearing appropriate footwear)
Escape Pain
ESCAPE-pain is a rehabilitation programme for people with chronic joint pain of the knees and/or hips, that integrates educational self-management and coping strategies with an exercise regimen individualised for each participant. It helps people understand their condition, teaches them simple things they can help themselves with, and takes them through a progressive exercise programme so they learn how to cope with pain better.
Robust evaluation shows that ESCAPE-pain:
Reduces pain
Improves physical function
Improves the psychosocial consequences of pain
Reduces healthcare and utilisation costs.
What treatments are there?
If you still have pain after trying self-help measures, your doctor may recommend the following treatments:
Physiotherapy
Steroid injections into the painful joint
Surgery, including joint replacement.
There is minimal strong evidence to support the use of joint injections in a knee with normal age related changes, especially as the effects have a short-term effect. You should discuss this option further with your health care professional especially as there are some side effects and adverse risks involved with a steroid injection.
Recent studies have shown that in the early stages of knee OA surgery should not be used. It has frequently shown poor outcomes and in many cases has sped up the progress of the OA.
What can Physiotherapy do for me?
Physiotherapy, which encompasses exercise and education, is the best and most effective method to help manage your pain and help you return to your normal function. Your physiotherapist will help you identify any issues through their initial assessment and will help you with a specific individualised exercise program.
Your rehab plan may aim to address the overload at the knee by:
Reducing pain
Strengthening weak structures (above and below the knee)
Correcting the way you move
Improving your movement control
Stretching tight structures
To achieve your specified goals as discussed with your physiotherapist, you will be required to attend regular physiotherapy appointments and most importantly continue your exercise program at home.
Pain Management
After an injury you may have heard about RICE (rest, ice, compression and elevation) when managing an injury. However, rest can be harmful and inhibits recovery. Recent research has now advised that we use the acronym POLICE.
Protection
Optimal-Load
Ice
Compression
Elevation
The key term is Optimal-load, this replaces Rest. You may need to speak to your physiotherapist to discuss what your optimal load might be as it is specific to you but will help speed up your recovery process.
Flare ups
An increase in pain or ‘flare up’ is common with knee osteoarthritis. The key is to manage this effectively and efficiently. By using POLICE this can help reduce the initial pain. During a flare up managing your optimal load is important. You may need to reduce the stresses at the knee or reduce the amount of exercises and daily activities that you do. Over time, gradually increase your activity back to previous levels.
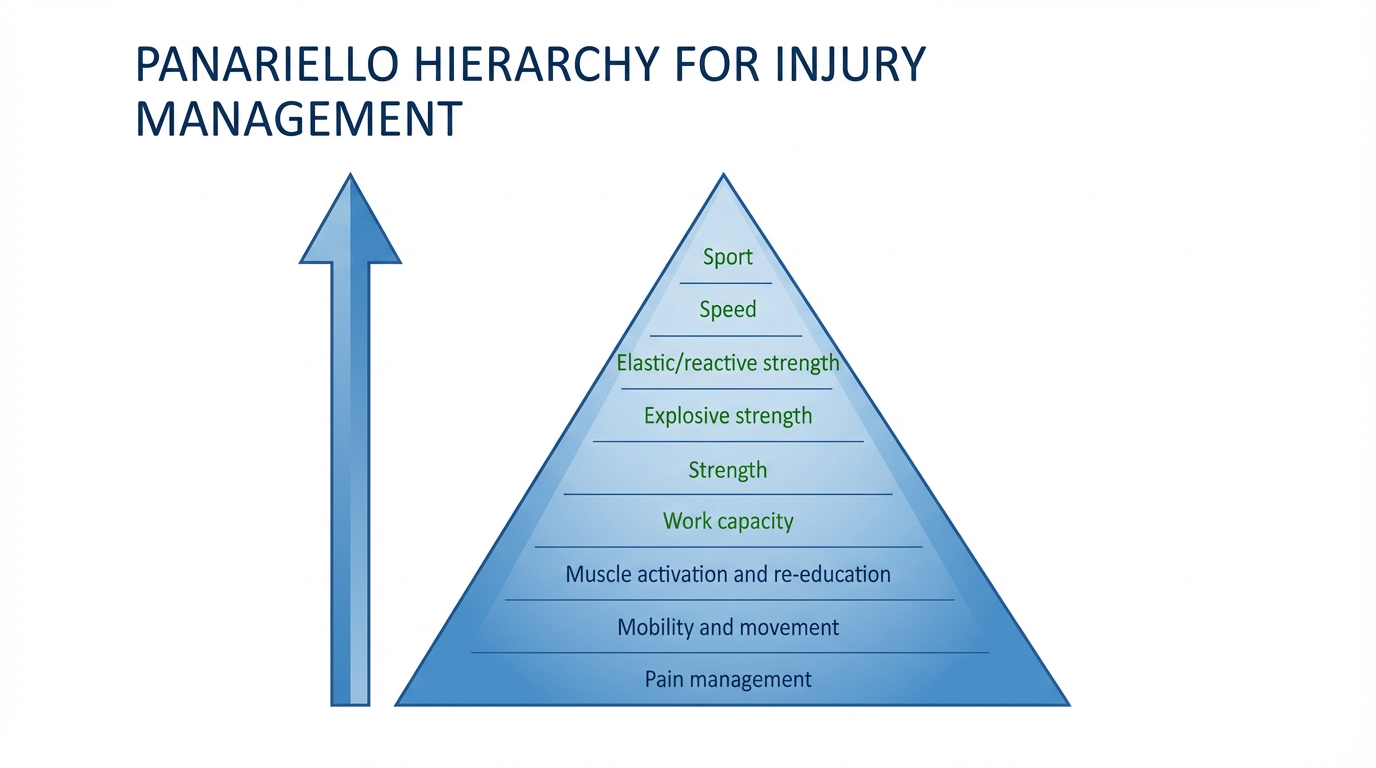
You can discuss optimal load with your physiotherapist. Below is a table which shows what type of exercises should be used and a hierarchy for return to normal activities. We will follow this pathway in the exercises later on. They often over lap and sometimes one exercise can have two goals, you can discuss this with your healthcare professional further.
Exercise
As mentioned exercise is one of the first lines in management in a knee with normal age related changes. It is key to ensure you continue to function well by maintaining strength, range of movement, fitness and joint health with increasing evidence showing that exercise can protect the joint from further changes.
The current physical guidelines for activity in the UK are:
75 minutes of intense exercise per week
150 minutes of moderate exercise per week
2 resistance training sessions per week.
When beginning an exercise program, it’s best to start slowly. Some examples of low-impact, non-strenuous exercise include:
Stationary bike
Using a stationary bike on an easy setting allows you to slowly build your strength. Using the bike in your home allows you to avoid traffic and stop when you feel strained. A bike is a more favorable choice than walking due to the less load going through your knee. If you struggle to ride a bike, a set of home pedals is also a good option to get your knee moving.
Water exercises
Freestyle swimming provides a moderate workout. Walking in water up to your waist lightens the load on your joints while also providing enough resistance for your muscles to become stronger. This can greatly improve pain and daily function of the knees.
Yoga
Regular yoga can help improve flexibility of the joints, strengthen muscles, and lessen pain. Some yoga positions can add strain to your knees, so if you feel discomfort, ask your instructor for modifications. A class for beginners is a good place to start.
Tai chi
The slow, fluid movements of tai chi may relieve arthritis pain and improve balance. Tai chi is a natural and healthy stress reducer as well.
Walking
If you have balance problems, using a treadmill (with no incline) allows you to hold on. Walking at a comfortable pace — whether it’s indoors or outdoors — is an excellent low-impact exercise.
Muscle strengthening exercises
Once you have improved mobility and movement the next stage is to develop strong muscles to help take pressure off your knee joints and help improve balance. We will guide you through the process in the next stage of this web page.