Femoroacetabular impingement (FAI), Hip Impingement
Hip impingement also known as femoroacetabular impingement occurs when there is abnormal contact between the hip’s bones. Anyone can have hip impingement although it is often diagnosed in active people in their 20s, 30s and 40s. This information page is designed to help you understand your diagnosis and by following these exercises, we will guide you through each step on your return to activities of daily living or any sporting goals you have.
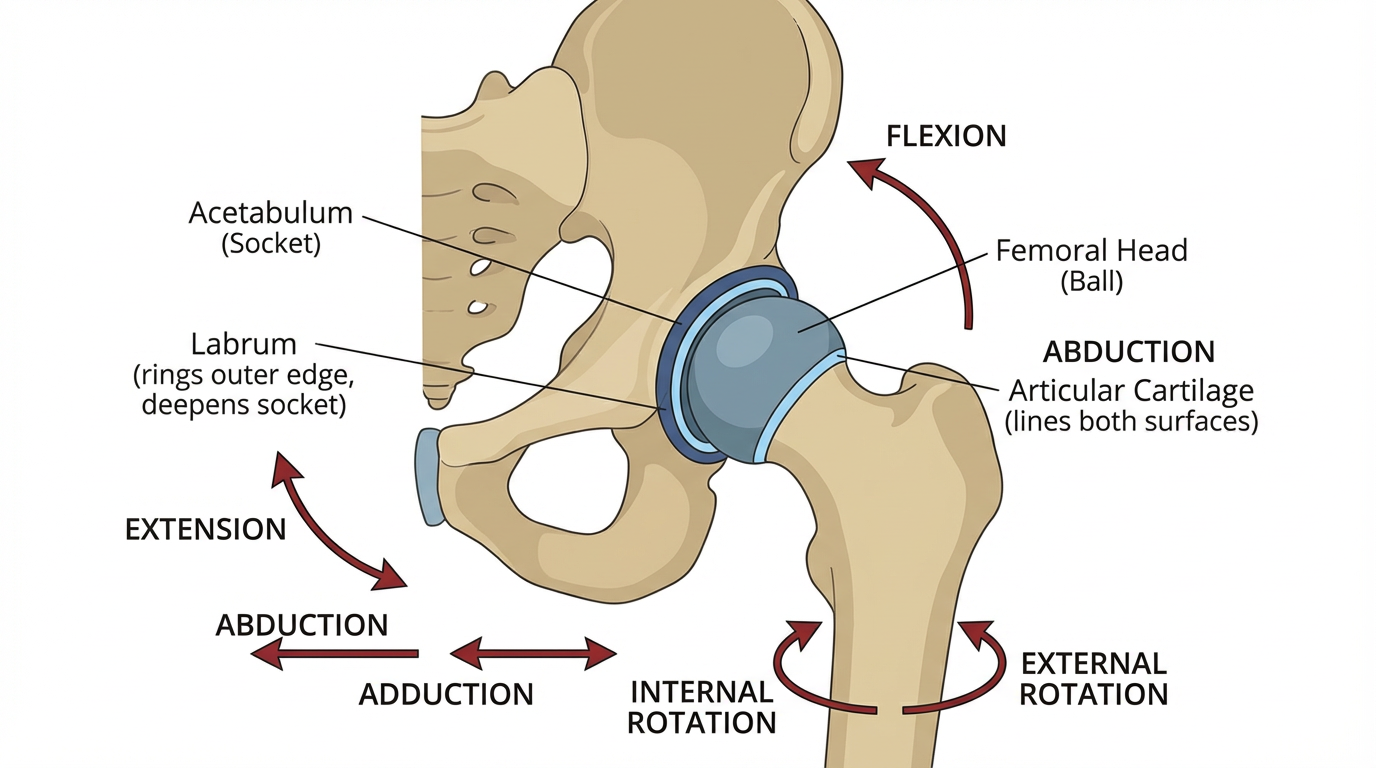
Hip Anatomy
The hip is a ball-and-socket joint.
The ball (femoral head) is the rounded top of the femur, commonly known as the thighbone.
The socket (acetabulum) is located in the pelvis.
The femoral head fits into the socket. The ball-and-socket anatomy allows the leg to move forward, backward, and side-to-side. It also allows for internal and external rotation (pointing the toes inward and outward).
Cartilage helps stabilise the hip joint and facilitate hip movement.
Articular cartilage. Both the femoral head and the acetabulum are lined with a strong, slippery material called articular cartilage. This cartilage allows the surfaces of the ball and socket to glide against each other during hip movement.
Labrum. Another piece of cartilage, called the labrum, rings the outer edge of the acetabulum. The labrum deepens the socket, making the hip joint more stable, and its elasticity allows for flexibility.
Understanding hip anatomy is necessary to understanding hip impingement and its possible long-term effects.
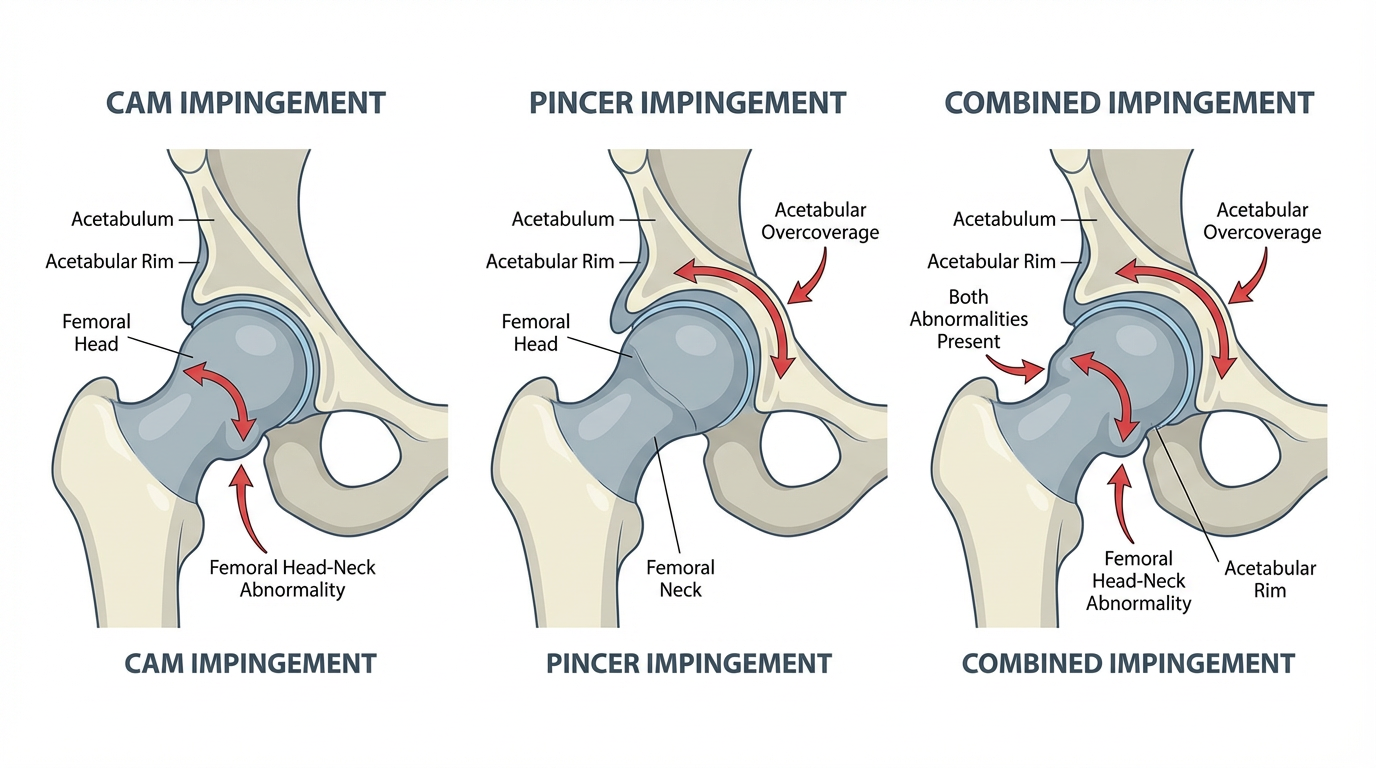
Types of Hip Impingement
In most active adults, hip impingement is caused by abnormal bone growth. The abnormal growth can occur near the femoral head, the acetabulum, or both. The location of the abnormal growth determines what type of impingement occurs:
Cam
A cam impingement occurs when excessive bone grows at the edge of the femoral head, where it meets a part of the femur called the femoral neck. The excessive bone growth forms a bump, which can do one or both of the following:
Prevent the femoral head from fully rotating in its socket.
Rub against the cartilage located inside the hip’s socket, causing damage to the cartilage.
Cam impingement is most common in young men.
Pincer
A pincer impingement occurs when excessive bone grows at the edge of the hip’s socket. The excess bone creates an overhang, making the socket too deep in certain places. The excessive bone tissue can:
Prevent the femoral head from rotating in its socket.
Cause the hip’s labrum to become pinched.
Pincer impingement tends to be most common in middle-aged women.
Combined
Many people have both cam and pincer hip impingement.
Medical imaging to determine which type of hip impingement a patient has.
-
In addition to hip pain, a person with hip impingement may experience:
Loss of range of motion, particularly when rotating the hip inward or moving the leg toward the centerline of the body.
Stiffness around the hip, making movements slower or more difficult.
Trouble going up stairs. Changes to the hip’s range of motion may change a person’s natural gait while climbing stairs.
Decreased muscle strength around the hip.
A loss of balance. Balancing on the affected leg may be more difficult than balancing on the unaffected leg.
Limping. In moderate to severe cases of hip impingement, hip pain and other symptoms may cause a person to walk with a limp.
Most people experience a loss of range of motion in the hip. The other symptoms may or may not occur depending on the severity of the impingement and how long it has gone untreated.
-
Physiotherapy is the best and most effective method to help manage your pain and help you return to your normal function. The main aim of physiotherapy through exercise is to improve musculature capacity to optimise lower limb mechanics and activate muscles around the hip to build strong pelvic/core control. This can reduce pain and improve your general function. Your physiotherapist will help you identify any issues through their initial assessment and will help you with a specific individualised exercise program.
Your rehab plan may aim to address the overload at the hip joint by:
Reducing pain
strengthening weak structures (deep, intermediate and superficial hip muscles)
Correcting the way you move
Improving your movement control
Stretching tight structures by improving soft tissue flexibility, length and mobilise the hip joint
To achieve your specified goals as discussed with your physiotherapist, you will be required to attend regular physiotherapy appointments and most importantly continue your exercise program at home.
-
After an injury you may have heard from someone before about RICE (rest, ice, compression and elevation) when managing an injury. However, rest can be harmful and inhibits recovery. Recent research has now advised we use the acronym POLICE.
Protection
Optimal-Load
Ice
Compression
Elevation
The key term is Optimal-load, this replaces Rest. You may need to speak to your physiotherapist to discuss what your optimal load might be as it is specific to you but will help speed up your recovery process.
Flare ups
An increase in pain or ‘flare up’ is common with hip impingement. The key is to manage this effectively and efficiently. By using POLICE this can help reduce the initial pain. During a flare up managing your optimal load is important. You may need to reduce the stresses at the hip, reduce the amount of exercises and daily activities that you do. Over time gradually increase your activity back to previous levels. You can discuss optimal load with your physiotherapist.
How long will it take to get better?
Unfortunately, there is not definite answer to this question. There are no quick fixes and it requires active participation from the patient throughout the process.
We would, however, expect to see improvements within 3-6 months especially if the patient continues to maintain their specific exercise program.